Sarah’s Story
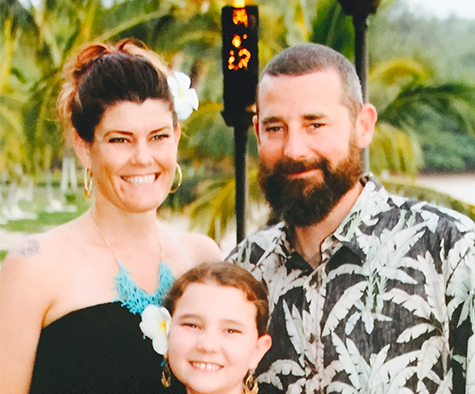
Sarah’s world was turned upside down in 2018 when her 45-year-old husband – and father to her 13-year-old daughter – was diagnosed with Stage IV rectal cancer. As a devoted care partner, she has learned the sheer power that advocacy and education play in supporting those on a cancer journey and helping us to maximize time with our loved ones.
Love at First Sight
Nathan was originally from Massachusetts, but he and Sarah met in Vail, Colorado, when they were both in their early 20s. Nathan worked in building maintenance at a local hotel, and Sarah worked in a coffee shop. He came in for a cup of coffee, and in Sarah’s words: “the rest was history.” They were together for almost 25 years.
“Nathan was charismatic. He got along with everyone, and everybody felt very comfortable around him. Nothing ruffled him, and he had a very calm energy. He was also extremely smart—he would read books about things like the Ottoman Empire for fun. Nathan would watch complex shows like Game of Thrones and remember all the characters’ names and where they were from and their lines of descent. He could talk about anything—he was just such an easy person to be around.”
Initial Symptoms, Diagnosis, and Treatment
Nathan’s cancer journey started in October of 2017, when he began experiencing constipation. He went to his primary care doctor, which set off an alarm for Sarah because he wasn’t someone who would typically go to the doctor for minor things. For the three months that followed, Nathan’s doctor had him try things like eating more roughage and taking laxatives, but they didn’t help. Nathan kept going back to his doctor, and she kept dismissing his symptoms. It wasn’t until he started passing blood that his doctor sent him for a sonogram. The sonogram revealed a 10-centimeter mass on his liver.
“I was at work when Nathan called me to tell me about the sonogram results. When I got home, I just broke down. I absolutely lost my marbles. My mom had died of breast cancer three months earlier, and I had walked this journey with her. Even before we had the details about Nathan’s cancer, I knew the size of the animal we were dealing with.”
After a biopsy, Nathan was diagnosed with stage IV rectal cancer. The cancer had started in his rectum and had metastasized to his liver and lungs. Nathan’s oncologist at the time did not recommend surgery because of the size of his liver tumor, and instead started him on chemotherapy.
Gathering Information
Sarah jumped into survival mode immediately after receiving Nathan’s diagnosis; it was all she knew how to do. She felt like she was in a state of shock, but rather than being numb from it, she got proactive and began searching for answers.
“I had just lost my mom—I couldn’t lose Nathan, too.”
She found COLONTOWN, an online community that brings together thousands of people with colon and rectal cancer, survivors, and care partners – and organizes them into groups based on their type of cancer, stage of disease, interest in clinical trials, etc.
“Connecting with these people was so meaningful to me because they were the only ones who really got what I was going through.”
Through COLONTOWN, Sarah started learning about different lines of treatment and testing. She also heard about people who were advocating for themselves with their oncologists.
“This was very eye-opening to me. At first, I accepted what Nathan’s oncologist said. But after connecting with others, I realized I had to do some of the work myself in terms of learning about options so I could ask the doctor questions.”
Guardant360 Experience
Nathan had received fluorescence in situ hybridization, or FISH testing, which looks for certain genetic abnormalities associated with cancer. The testing showed abnormalities in HER2 gene activity. Sarah and Nathan learned that HER2 amplification, which is fairly common in breast cancer, was not as common in rectal cancer, so Sarah joined a HER2 COLONTOWN group to learn more about it.
At Nathan’s next oncologist appointment, Sarah brought up questions based on what she had discovered in the HER2 group. She asked if Nathan qualified for any clinical trials, and she also asked about the Guardant360 test, which she had heard about in her group. The oncologist said the Guardant360 test wasn’t necessary and that there were no clinical trials available for Nathan.
Sarah wanted to be sure, so she asked her for a referral for a second opinion at an out-of-network comprehensive cancer center. Nathan’s oncologist wouldn’t give it to her, but Sarah wasn’t going to take no for an answer, so she decided to pay out-of-pocket for a second opinion. She’s grateful she did.
“When we met with the second-opinion oncologist in October of 2019, one of the first things he said was, “I’d like to do a Guardant test.” I felt very validated by that. Based on what we learned from the second opinion and the Guardant360 test, we changed our health insurance and switched to a different oncology team.”
Opening Doors and New Directions
According to Sarah, the results of Nathan’s Guardant360 test opened up new treatment opportunities for him. The test uncovered information about the genetic profile of his cancer cells, which allowed his new oncologist to begin targeting Nathan’s treatment more precisely.
By this time, Nathan had exhausted two chemotherapy regimens. He was starting to go downhill, and his former oncologist was considering last-line treatments. But his new oncologist decided to treat him with an investigational therapy under the Right to Try Act that targeted his HER2 amplification. His new oncologist also told Sarah and Nathan that she would continue ordering ongoing Guardant360 testing, since mutations can change over time.
Nathan started to feel better as soon as he started targeted therapy. During his treatment, his oncologist did the Guardant360 test two more times, and each time, she adjusted his treatment based on its findings.
“Nathan lived two more years after having that first Guardant360 test. During those two years, he bought a car for our daughter who had turned 16 and had started driving. He attended many of her volleyball games. And he continued working until about two months before he died, which was important to him. He enjoyed his work, but more than that, work gave him a sense of control. That’s something that gets ripped away from you very quickly with a cancer diagnosis.”
Unfortunately, in July of 2021, Nathan’s battle with rectal cancer came to an end.
“I didn’t get the outcome I wanted. Nathan wasn’t cured. But thanks to testing with Guardant360, his doctor was able to create a treatment plan specific to Nathan and his condition. I believe he had two more good years than he might not otherwise have had. I’m grateful for that.”
Advice for Patients and Care Partners
In reflecting on her time as a care partner, one piece of advice Sarah would like to share with others is to not be afraid to seek second opinions, or even third opinions.
“Too many of us are conditioned to do what our doctors say without question. We’re taught that it’s offensive to challenge a doctor, and that it would hurt their feelings to ask for a second opinion. But when it comes to your life, you cannot be afraid. Any good oncologist welcomes a second opinion. If you’re seeing a doctor who has a problem with it, they are probably not someone you want on your care team.”
Additionally, if you are a care partner, being the one to question the doctors, and even challenge them – if necessary – means your loved one doesn’t have to do it. Nathan and Sarah established a dynamic where he sat back and focused on treatment and letting his body recover, and she did the research and the advocating. That worked well for them, she shared.
Sarah also recommends that whether you’re a patient or a care partner, you need to make sure you have support and can find a group of people who are going through something similar. Not only can these other people support you, she says, but they can also share information and advice on next steps and preferred oncologists, surgeons, and treatment centers.
Finally, she reminds others to not be afraid to speak up to their oncologists about genomic testing.
“If you have a doctor who has done things a certain way for a long time, they may not be as excited or open to trying something different. Speak up, and ask for testing.”
Finding Purpose and Hope
Sarah left her job as a teacher during Nathan’s treatment. She didn’t want to risk exposing herself to COVID and passing it along to him. She decided to start volunteering instead. The woman who started COLONTOWN was launching a patient-powered cancer learning community site called One Cancer Place, and Sarah offered to help out.
Today, Sarah supports One Cancer Place with organizing various types of in-person and online learning experiences, including symposiums in which leading oncologists share information and answer questions from patients and care partners.
“When a diagnosis plunges you into the world of cancer, you have to learn so much in such a short amount of time. Our goal is to provide information patients and their care partners need. Connecting patients with the opportunity to learn is so meaningful to me.”
Through her advocacy work, Sarah is seeing that more oncologists are recognizing the benefit of patient education and advocacy – and realizing that when patients and care partners are educated, they’re better able to participate in their care and make informed choices.
This gives her hope.
“I want everyone to know that understanding and learning about a diagnosis and treatment options is the best thing you can do. We all want to be here for as long as we can. Educating ourselves is one way we can go about helping to make that happen.”